Apart from the potential curse of Lange Covid, people who have had the SARS-COV-2 virus are more likely to develop high levels of biomarkers for brain proteins linked to Alzheimer’s disease, scientists report in a new study.
The average estimated effect of the virus on beta -amyloid proteins was comparable to the effect of four years of aging, researchers found.
The difference was most pronounced in patients who were admitted to the hospital with severe COVID-19, found the study, or in patients with underlying risk factors for dementia, such as high blood pressure.
These results indicate another treacherous effect of COVID, the researchers write, which suggests that even mild or moderate cases can speed up biological processes that promote the accumulation of beta -amyloid proteins, which has previously linked research to Alzheimer.
However, there are important comments to notice. Firstly, this was an observational study, so it can establish a correlation but no causal connection.
And even if Covid increases the risk of these biomarkers, we do not know whether that effect would be unique for SARS-COV-2, or whether it can be caused in the same way by other pathogens such as the flu.
The blood biomarkers used in this study are also fairly new, the authors acknowledge and reliably reliable as clinical aids.
Given the devastating effects of Alzheimer’s and its uncertain origin, instructions such as these valuable pieces of an urgent puzzle can be.
This fits in with research from the past that suggests that some types of infections can increase the risk of Alzheimer’s for some people, says neuroscientist Eugene Duff from Imperial College London.
“Our findings suggest that COVID-19 can manage changes that contribute to neurodegenerative disease,” says Duff. “We think that this can be due to the inflammation caused by the disease, although how this inflammation can influence the brain and changes in amyloid is not yet completely clear.
“We cannot say that catching the SARS-COV-2 virus directly causes these changes, or if this is the case, by how much a single episode of infection increases a person’s risk,” he notes.
“But our findings suggest that COVID-19 can increase the risk of Alzheimer’s in the future-as has been suggested in the past for other types of infections, especially in people with existing risk factors,” he says.
Alzheimer is a cruel and mysterious neurodegenerative disease that can gradually destroy the memory and cognitive skills of a person. It is the most common form of dementia, a group of brain disorders that affect more than 55 million people worldwide.
According to the World Health Organization, around 10 million new cases of dementia are diagnosed every year, which estimates that Alzheimer can be good for two -thirds of all cases.
Despite the prevalence, Alzheimer’s is still dressed in mystery. A lot of attention is focused on beta -amyloid plaques, although it is unclear what role that playing and whether they cause the disease or vice versa.
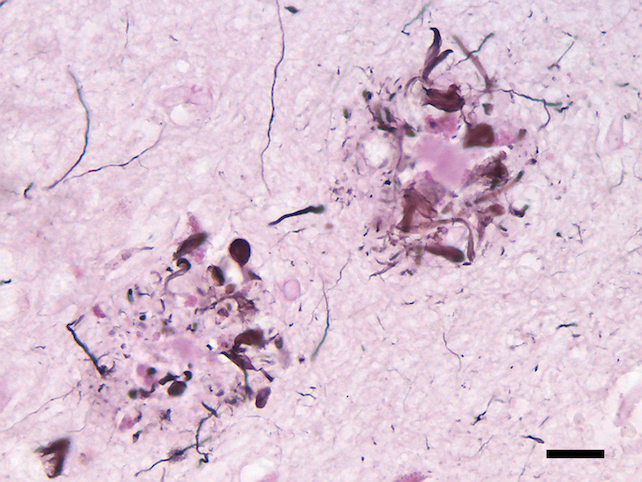
Beta -Amyloid proteins are common in the body and serve a series of purposes. Their accumulation in lumps, or plaques, is what is disturbing.
These plaques are highly associated with Alzheimer’s, and although their role remains cloudy, they can cause symptoms of the disease by damaging neurons in the brain, the authors of the study note.
Given the uncertainty, it seems wise to pay attention to at least if something correlates with suspected Alzheimer’s biomarkers – in this case proportions of different forms of beta -amyloid.
Duff and his colleagues looked at data from 1,252 participants in the British Biobank, ranging from 46 to 80 years old. This includes data collected, both before and after confirmed SARS-COV-2 infections.
They compared biomarkers of former COVID patients with patients from participants who have similar properties, but no proof of previous infections.
People with a COVID history were more likely to have specific changes in blood proteins that previously linked research to beta-amyloid pathology in the brain, according to the study.
The change of change reminded of that of a genetic variant known as Apoe4, an established risk factor for Alzheimer’s disease, the researchers noted.
The change was also more dramatic in people who were admitted to the hospital for Covid – and for people with well -known Alzheimer’s risico factors, such as hypertension.
“We have long suspected a connection between infectious diseases and the progression of neurodegenerative diseases – both with viral diseases such as herpes and influenza, and with some chronic bacterial infections,” says senior author Paul Matthews, a neurologist at the UK Dementia Research Institute on Imperial College London.
“The latter analysis suggests that SARS-COV-2 infection may be one of these medical expenses, especially with those with underlying risk factors,” he says.
“Ultimately, the more we know about factors that contribute to the risk of dementia – whether they are directly under our control, such as lifestyle or diet, or can be changed by vaccines or asked the prevention of dementia,” he adds.
The study was published in Nature Medicine.



